Infertility Treatment and Services
Efficiency Practice Model for Infertility Treatment
Dr. Craig does not push high-tech options such as IVF or Donor Egg onto patients, but instead reviews all low, medium, and high-tech options, and recommends the appropriate level of treatment to maximize the chance of pregnancy at the lowest cost.
He works with patients at the treatment level that is most comfortable and affordable for them. In fact, 74% of treatment cycles performed at FTC include ovulation induction and intrauterine insemination (IUI fertility treatment) — low-tech treatments requiring less medication and fewer monitoring appointments with a lower cost. (Scroll down to view each level of treatment)
TREATMENT PLANNING

When you meet with Dr. Craig, Kristen, Kristina, or Shannon for your initial consult, he or she will outline a diagnostic plan (an infertility work-up) based on your gender, your medical history, a physical examination, ultrasound, diagnostic labs, a hysterosalpingogram (HSG), and if necessary a semen analysis and/or diagnostic surgery.
It is important to understand if you have menstruation irregularities, ovulation disorder, PCOS, endometriosis fibroids, male infertility, etc.

Transvaginal Ultrasound
Paired with bloodwork, an ultrasound is used to count the antral follicles in the ovaries to help complete the picture and determine the status of your ovarian reserve, and which fertility procedures are appropriate.
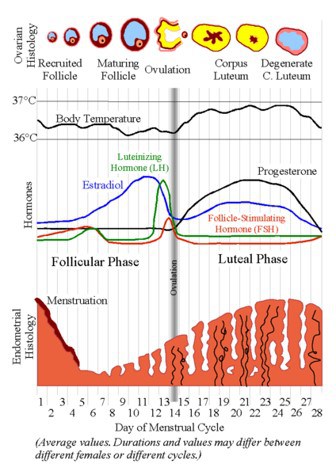
Testing Hormones that Control Ovulation and Embryo Implantation
We will evaluate LH (luteinizing hormone): stimulates the release of the egg from the follicles (ovulation), and Progesterone: stabilizes the uterine lining for implantation of a fertilized egg and supports early pregnancy. We may also test Androgens, Prolactin, and Thyroid.

Testing Hormones Indicate Ovarian Reserve
The ability for a woman to conceive is directly related to the number of eggs she has remaining in her ovarian reserve. We will test the following hormones: E2 (estrogen): stimulates the growth of the follicles and the production of fertile mucus from the cervix; also prepares the uterine lining for implantation of a fertilized egg, FSH (follicle-stimulating hormone): stimulates the development of the egg, and AMH (anti-Müllerian hormone): secreted by the small antral follicles found in the ovaries at the start of the cycle indicates the size of the ovarian reserve.
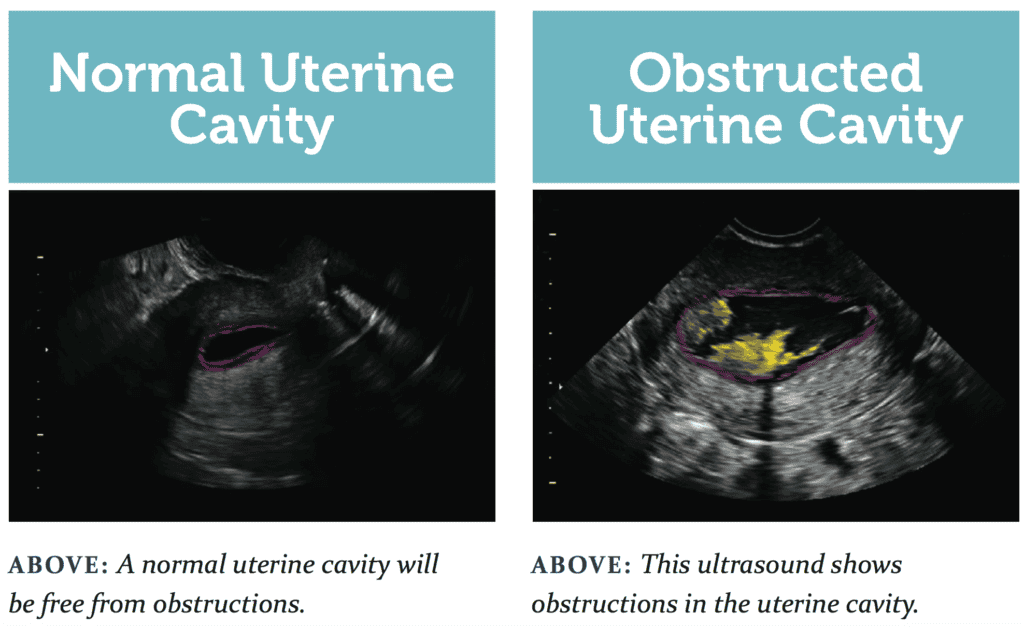
Sonohysterogram (SIS or SHG)
A sonohysterogram (SHG), also called a saline infusion sonogram (SIS) is a diagnostic procedure performed in our office to evaluate the uterus by injecting saline into the uterine cavity while performing an ultrasound. The saline helps create a clearer image of the uterine lining and structure, allowing doctors to detect abnormalities such as polyps, fibroids, or scarring. This non-invasive procedure is commonly used to investigate causes of abnormal bleeding, infertility, or recurrent miscarriages and is typically done with minimal discomfort.
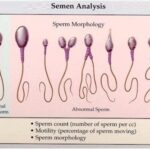
Semen Analysis
A semen analysis is a male fertility test that assesses the formation and maturity of sperm as well as how the sperm interact with the seminal fluid. A fresh semen sample (no more than a half hour old) is collected and then analyzed in a laboratory for a variety of different factors. In order for sperm to be able to fertilize an egg, it is necessary for seminal fluid to be of the correct consistency as well as for sperm to have maximum motility, ideal morphology, and sperm count. If any of these factors are revealed to be less than perfect in a semen analysis, male fertility may be compromised. Male infertility testing is an important part of making an accurate infertility diagnosis.

Male Factor Infertility Evaluation
A Male Factor Infertility Evaluation is a series of tests and assessments used to identify potential causes of infertility in men. The evaluation typically begins with a semen analysis to assess sperm count, motility, and morphology, followed by a physical exam and review of medical history. Hormonal testing, genetic screening, and imaging may also be conducted to detect issues such as low testosterone levels, blockages, or varicoceles. This comprehensive evaluation helps diagnose conditions that may affect fertility and guide treatment options such as lifestyle changes, medication, or assisted reproductive technologies including timed intercourse, IUI, or in vitro fertilization (IVF).

Hysterosalpingogram (HSG test)
Performed to check for blockage of the fallopian tubes or for growths in the uterus. About 15% of infertility is due to blocked fallopian tubes, which can interfere with egg fertilization or stop a fertilized egg from reaching the uterus. If your tube(s) is blocked, Dr. Craig can also attempt to open your tubes while performing the HSG, something not available at Imaging Centers or some other clinics. An HSG can also detect fibroids, polyps, adhesions and/or other growths or scarring in the uterus. The providers at FTC will perform and interpret.
LOW-TECH INFERTILITY TREATMENT
Timed Intercourse
One of the simplest treatment options for infertility and can be a starting point for many couples. When the cause of your infertility is unexplained, a cervical factor, or irregular or absent ovulation and you desire a low intervention treatment option, timed intercourse should be considered.
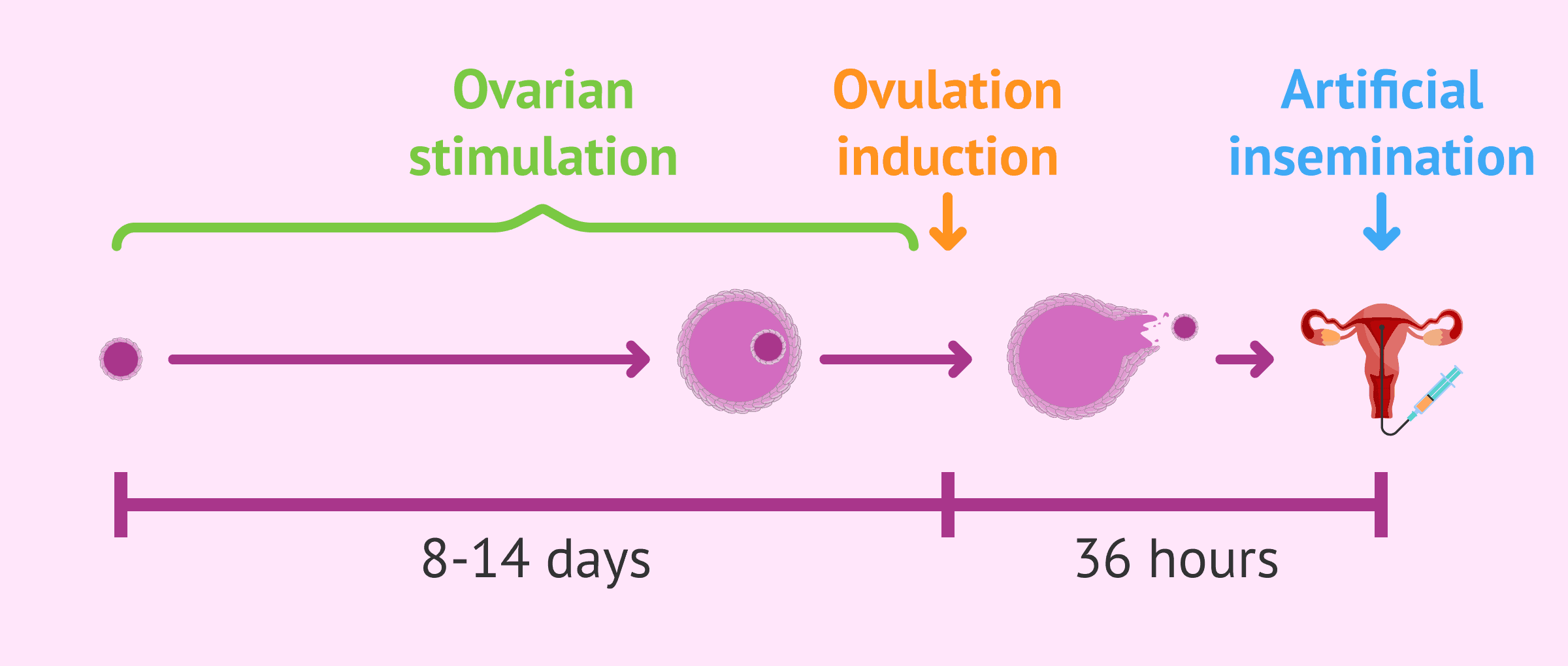
Ovulation Induction Infertility Treatment
For women who are not ovulating regularly, menstruation irregularities, the goal of treatment is to mature and ovulate a single egg—this is known as ovulation induction.
MEDIUM-TECH INFERTILITY TREATMENT
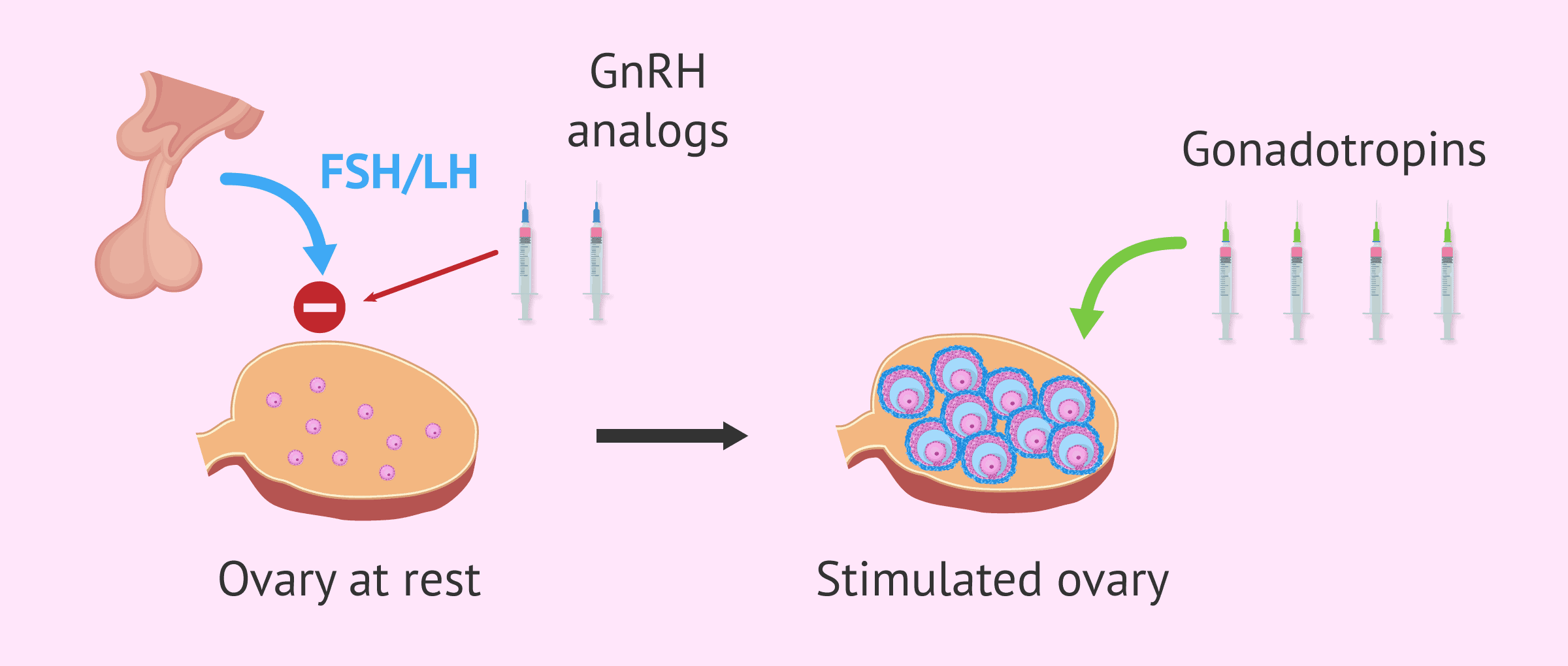
Superovulation Infertility Treatment
Some causes of infertility can be effectively treated with superovulation therapy. During superovulation therapy, the woman is treated with medications that increase the number of eggs she ovulates each month. At the appropriate time, intrauterine insemination is performed. Causes of infertility that can be treated with this therapy include ovarian dysfunction, infertility associated with endometriosis, cervical factor infertility, and infertility in which the exact cause cannot be identified. Superovulation therapy is also an effective addition in treating couples with needing male fertility treatment.

Sperm Freezing (Cropreservation)
Sperm freezing, also known as sperm cryopreservation, is a procedure used to preserve male fertility by collecting, freezing, and storing sperm for future use. It is often recommended for men facing urgent situations such as cancer treatment, military deployment, or other medical conditions that may affect fertility. By freezing sperm before chemotherapy, radiation, or surgeries that could impair reproductive function, men can retain the option of fathering biological children later in life. The frozen sperm can be stored for many years and used in assisted reproductive technologies like in vitro fertilization (IVF) or intrauterine insemination (IUI) when the individual is ready to start a family.
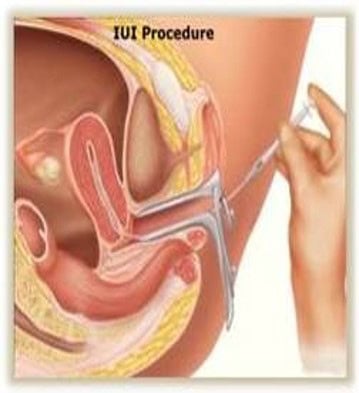
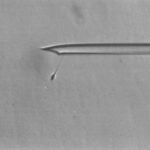
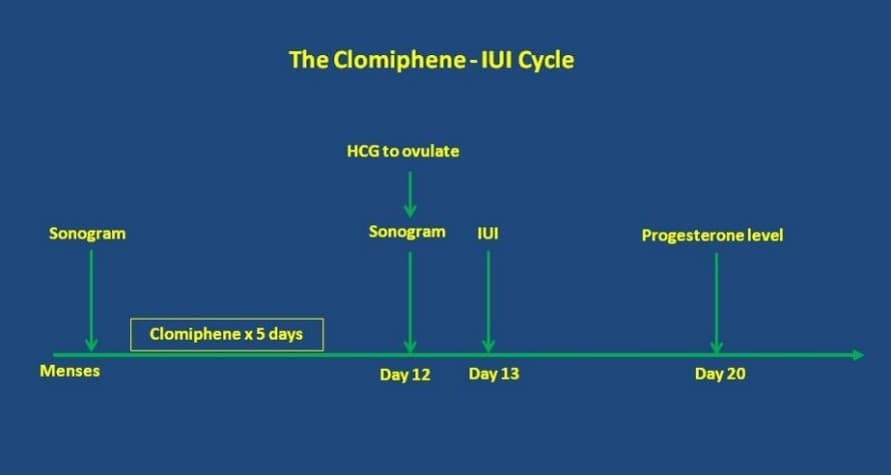
Intrauterine Insemination (IUI) also called Artificial Insemination (AI)
Artificial insemination is a low tech form of fertility treatment. It is generally used in two ways: natural and with ovulation induction. Couples who are experiencing fertility problems may be able to use IUI fertilization as a means to increase the likelihood of pregnancy. IUI fertility treatment is an in-office procedure and uses a specially prepared semen sample that has been obtained from the partner or donor. During artificial insemination, the sperm is placed gently in the uterus using a catheter carefully maneuvered through the cervix. IUI is considered a relatively painless procedure.
Donor Sperm IUI
You and your partner may elect to use donated sperm if the male partner has no sperm or very poor quality sperm, if he has undergone previous radiation or chemotherapy treatment, or if he has a genetic disorder that might be inherited. Donor sperm with IUI fertilization is also commonly needed by single women and same-sex female couples.
HIGH-TECH INFERTILITY TREATMENT
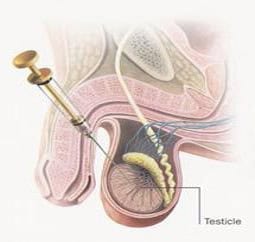
Sperm Aspiration and Extraction
Microsurgical epididymal sperm aspiration (MESA) and percutaneous epididymal sperm aspiration (PESA) are available for men with obstructed or absent ejaculatory ducts (i.e. unsuccessful vasectomy reversal, congenital absence of the vas deferens). Sperm are aspirated directly from the epididymis (the tiny collecting tubules next to the testes) for use in the ICSI procedure. The few drops of fluid may contain sufficient sperm to be frozen for several ICSI procedures. Testicular sperm extraction (TESE) is available for men with obstructions or ejaculatory problems that cannot be treated by any other method. Small samples of testicular tissue are obtained by needle biopsy and a few sperm are painstakingly dissected out of the tissue for use in the ICSI procedure.

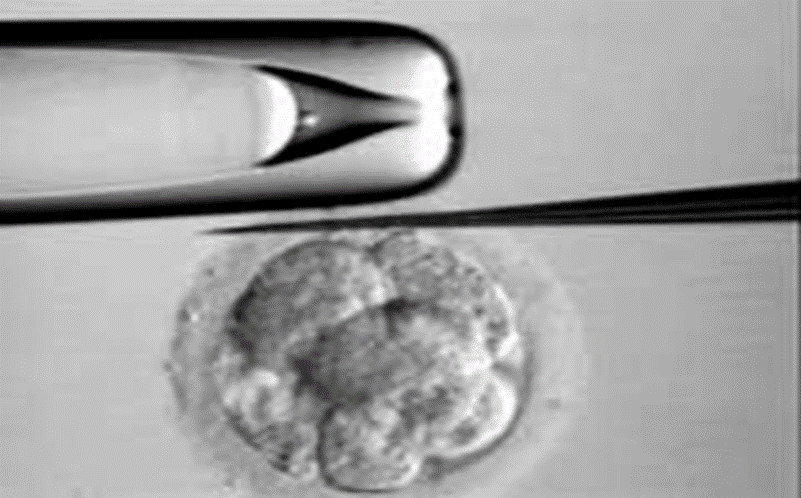
Preimplantation Genetic Testing (PGT) / Embryo Biopsy
Preimplantation Genetic Testing (PGT) is a technique that can be used during in vitro fertilization (IVF) to test embryos for a variety of genetic disorders. This procedure gives couples a chance to have a child unaffected by a genetic condition, without the uncertainty involved in becoming pregnant and using prenatal diagnosis. PGT involves harvesting cells from very early embryos after IVF or removing a polar body from an oocyte for analysis. This procedure is also used for gender selection.
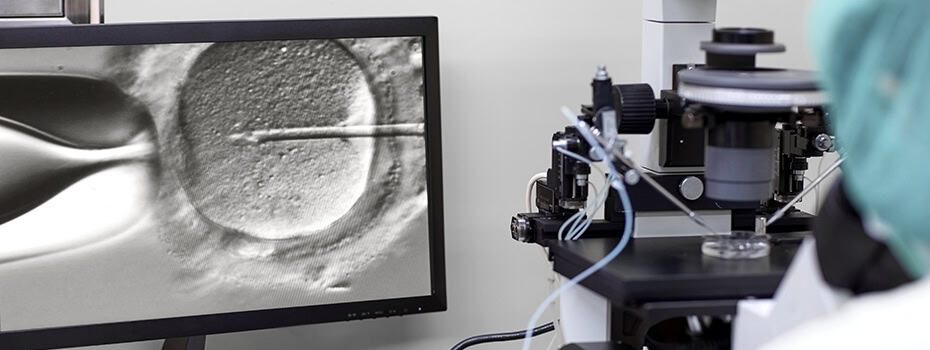
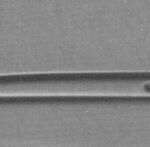
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a procedure used in conjunction with IVF in which a single sperm is inserted with a micro-needle into the cytoplasm of a mature egg. ICSI is often used if the male partner has very low sperm count, low sperm motility, or poor quality sperm. If fertilization occurs after ICSI, the embryo may then be transferred into the uterus.

In Vitro Fertilization (IVF) and Fresh Embryo Transfer (ET)
These are the most common ART procedures. They are used to treat infertility problems caused by adhesions, endometriosis, sperm antibodies, low sperm count, and unexplained infertility. The eggs are retrieved and then processed by the laboratory. They are isolated and mixed with properly processed sperm, and are then placed in an incubator where fertilization takes place. After oocyte fertilization, embryos that have developed satisfactorily are transferred into the uterus four days after egg retrieval.

Gestational Carrier
Our successful Gestational Carrier Program at Fertility Treatment Center was established for women who are unable to safely carry a pregnancy, women without a uterus, single men or gay men who want to build a family, or individuals/couples who are unsuccessful with other infertility treatments.

Frozen Embryo Transfer (FET)
FET is a cutting-edge infertility treatment. During FET, fertility specialists take frozen embryos and implant them in the patient’s uterus after the embryos have thawed. Reasons that couples choose FET include failed IUI procedures or the presence of extra embryos from an initial IVF cycle. In addition, any couple receiving donated embryos must undergo FET because all donor embryos are frozen for at least six months. A relatively non-invasive procedure, FET can be performed on women who have either controlled or natural menstrual cycles.
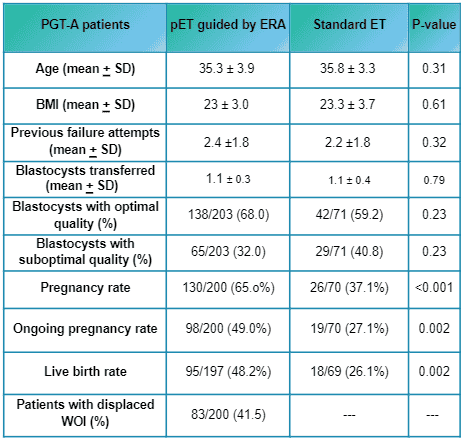
Endometrial Receptivity Analysis
The Endometrial Receptivity Analysis (ERA) is a diagnostic test used to evaluate the optimal timing for embryo transfer during in vitro fertilization (IVF). By analyzing a small sample of the uterine lining (endometrium), the ERA assesses whether the lining is receptive to an embryo at a specific point in a woman’s cycle. This personalized test helps identify the best window for implantation, improving the chances of successful pregnancy, especially for women who have experienced repeated IVF failures. The ERA can help tailor fertility treatments to maximize the likelihood of implantation and a healthy pregnancy.

Embryo Storage
Upon completion of your IVF treatment, any remaining embryos will need to be stored for your possible future use (or donation once your family building has completed). Cryopreserved or frozen embryos can potentially remain for an indefinite period of time at FTC’s cryobank.

Embryo Freezing (Cryopreservation)
Embryo Freezing (Cryopreservation) is the process of freezing embryos at a very low temperature so that they can be thawed and used later. IVF success rates with frozen embryos are very high at FTC because of our Day 4 ET (embryo transfer) protocol, which may allow couples multiple chances to achieve pregnancy from a single oocyte retrieval cycle. During a traditional cycle of IVF, we usually transfer 2 embryos to the uterus to maximize the chance of conception while minimizing the likelihood of multiple births. If pregnancy does not occur during the stimulated cycle, the frozen embryos may be thawed and transferred to the uterus during a spontaneous menstrual cycle. If conception does result from the initial stimulated cycle, cryopreserved embryos can be used later in an attempt to achieve another pregnancy.
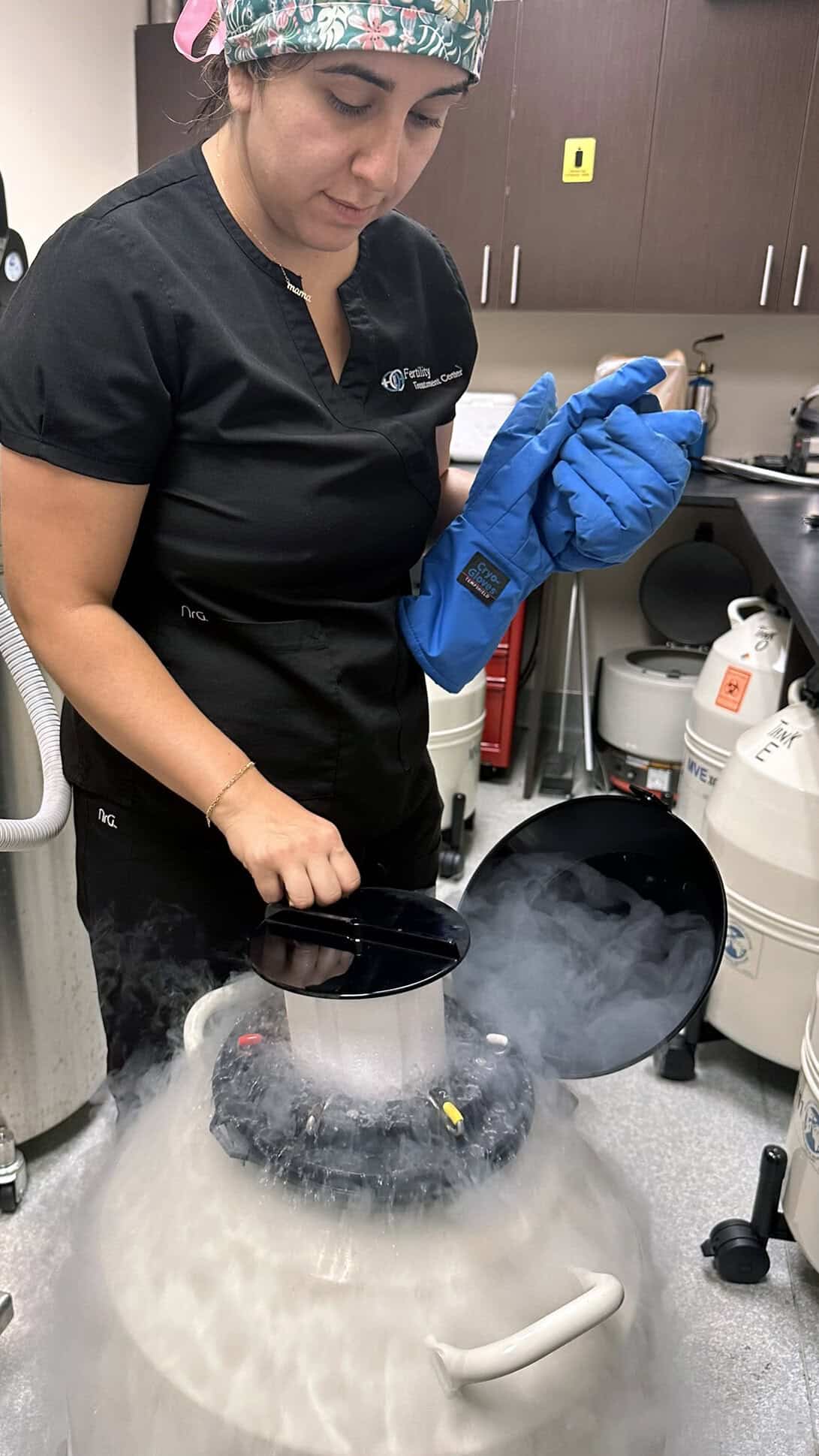
Egg Freezing (Oocyte Cryopreservation)
Egg freezing (oocyte cryopreservation) is a process where a woman’s eggs are extracted, frozen, and stored for future use. This fertility preservation technique is often used by women who want to delay childbirth for personal or medical reasons, such as undergoing treatments like chemotherapy. The process involves stimulating the ovaries to produce multiple eggs, retrieving and freezing them through vitrification, and storing them for potential fertilization later via in vitro fertilization (IVF). While success rates vary, especially with age, egg freezing offers an option to preserve reproductive potential for the future.
Donor Embryo Adoption
The Donor Embryo Adoption Program at Fertility Treatment Center is a method for you to achieve pregnancy at a much lower cost than In Vitro Fertilization.
Donor Egg
Seeking pregnancy through egg donation is an option for women who are over the age of 38 (advanced age increases the likelihood of egg abnormalities), suffer from premature menopause and/or poor ovarian function.
Egg donation involves a woman (a donor) “donating” her eggs so that another woman (a recipient) might be able to conceive. In egg donation, in vitro fertilization (IVF) is performed in the usual manner, except that the donor may receive fertility medications to stimulate the production of multiple eggs in her ovaries. At the same time, the recipient may also receive medications so that her cycle mirrors the cycle of the donor and her body is prepared to receive the embryo. The egg is then fertilized in a laboratory and the embryos are implanted in the recipient’s uterus. The success rate for couples undergoing in vitro fertilization (IVF) with egg donation — even when a woman is over age 40 — is approximately the same as the success rate of IVF in young women.
Generally, egg donation may be an option for a woman if she:
- Is older and has not succeeded with other therapies.
- Has reached menopause prematurely.
- May carry a genetic disorder that may have been determined through blood testing.
- Has experienced unexplained and repeated miscarriages.
Assisted Hatching
Assisted Hatching is a process used to aide the embryo to emerge from its covering prior to implantation in the uterus. In some cases, particularly as women age, the membrane hardens which can interfere with the natural hatching process.