Evaluation & Diagnosis


FTC offers fertility evaluation & infertility diagnosis of all aspects of reproductive care.
Infertility is generally defined as the inability of a couple to conceive a child after one year of unprotected sexual intercourse, the time in which about 90% of couples succeed. When a female is in her 20s, the average time to pregnancy is six months. This time frame reflects not only the limited few days in the middle of a woman’s menstrual cycle when she ovulates and conception is possible, but also the fact that most conceptions do not survive beyond early embryonic development and are lost before a woman’s next menstrual period. In addition, about 15% of couples with a clinical pregnancy go on to a spontaneous miscarriage. The female partner’s reproductive age is also an important determinant of the man’s ability to initiate pregnancy since the length of time required to establish pregnancy increases progressively with advancing maternal age. Fertilization of the egg is more difficult and early pregnancy loss is more frequent as a woman becomes older. Age is just one of a number of factors to consider when evaluating and diagnosing infertility causes.
What are the fertility options?
After Dr. Craig has reviewed your past medical history and performed a detailed physical examination, he’ll present a variety of options for you and your partner based on your individual needs. Some of those options may include:
- 1. Additional Testing
- 2. Ovulation induction medications
- 3. Intrauterine insemination
- 4. In vitro fertilization.
- 5. Donor egg or donor embryo.
- 6. Surgical intervention.
Armed with excellent information from the initial testing and exams, and with your input, Dr. Craig and the Staff at FTC will help you find the perfect plan to complete your family.
Infertility Evaluation Diagnosis topics include
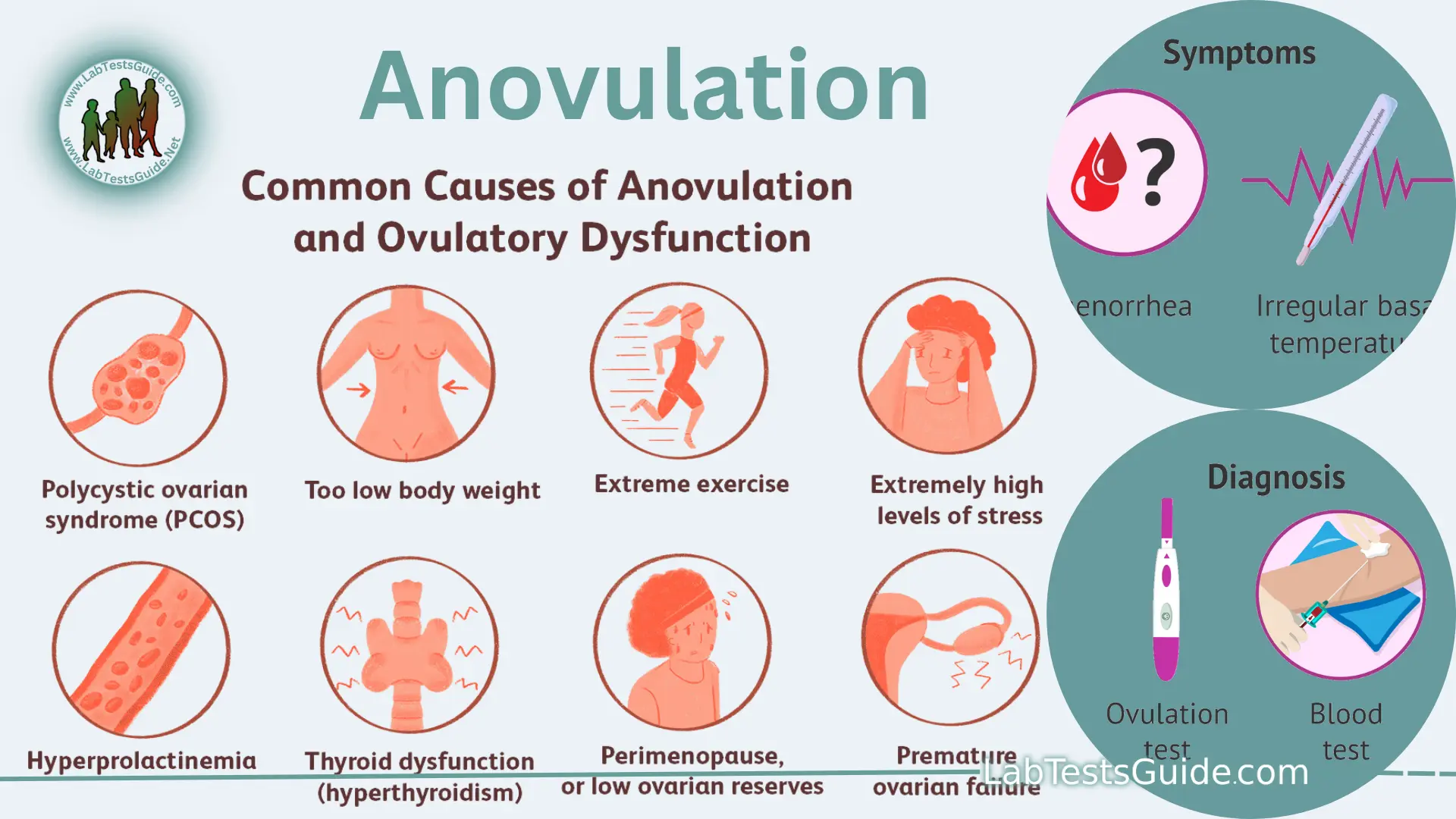
A disorder in which eggs do not develop properly, or are not released from the follicles of the ovaries. Women who have this disorder may not menstruate for several months. Others may menstruate even though they are not ovulating. Although anovulation may result from hormonal imbalances, eating disorders, and other medical disorders, the cause is often unknown. Women athletes who exercise excessively may also stop ovulating.
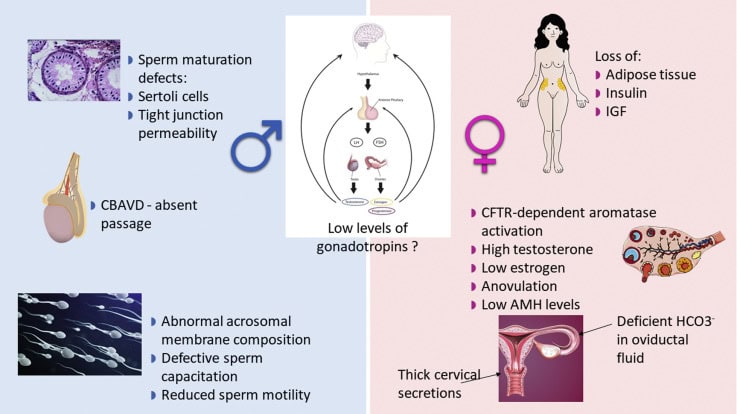
Cystic fibrosis patients often have missing or obstructed vas deferens (the tubes that carry sperm) and hence a low sperm count.
Diminished Ovarian Reserve is one of the more difficult diagnoses that a patient can have. That is because such patients are much more difficult to help to achieve pregnancy since the normal tools to achieve pregnancy don’t work as well. Some patients will likely have at most a few years of potential fertility left, so the situation is urgent. Some may have limited or no fertility left, but the process of finding this out, at times, involves a process of trial and error.
A woman is born with one to two million eggs. Although she will only ovulate three to four hundred of them, the rest will essentially wither away until there are none left. She will then be menopausal. Most of the time, the eggs are in a protected state with a small group of them constantly being released from this protection. We do not know what causes the ovary to change the status of these eggs, so we refer to it as a women’s biological clock. Those eggs that have left this arrested state will go on and ovulate provided they receive optimal hormonal stimulation. If they don’t get this stimulation, they soon undergo an actively defined degeneration (called apoptosis).
One way of defining decreased ovarian reserve is when a woman has fewer than 25,000 eggs in her ovaries. Statistically, this occurs around age 38. Fertility is still present until around 42 years old and, for most women, therapy to achieve pregnancy is still a reasonable thing to do. Menopause (no eggs) occurs around age 51. However, these numbers are only averages and these events have a distribution around these averages. For example, many women don’t experience menopause until well past age 51. Similarly about 10% of all women will have decreased ovarian reserve by age 32. In a practice such as mine, where women are self-selected to come here on the basis of not being able to get pregnant, the incidence of decreased ovarian reserve is even higher.
Women with certain histories need to be especially concerned about their reproductive potential. Of greatest concern is a family history of early menopause, certain chemotherapies, and pelvic radiation. Also of concern are a history of (significant) pelvic surgery, pelvic infection, severe endometriosis, and smoking (dose and duration related).
FTC performs a complete assessment for those patients at risk for diminished ovarian reserve, and does not exclude these patients from its practice nor have them pay more, as other practices due, because of their situation.
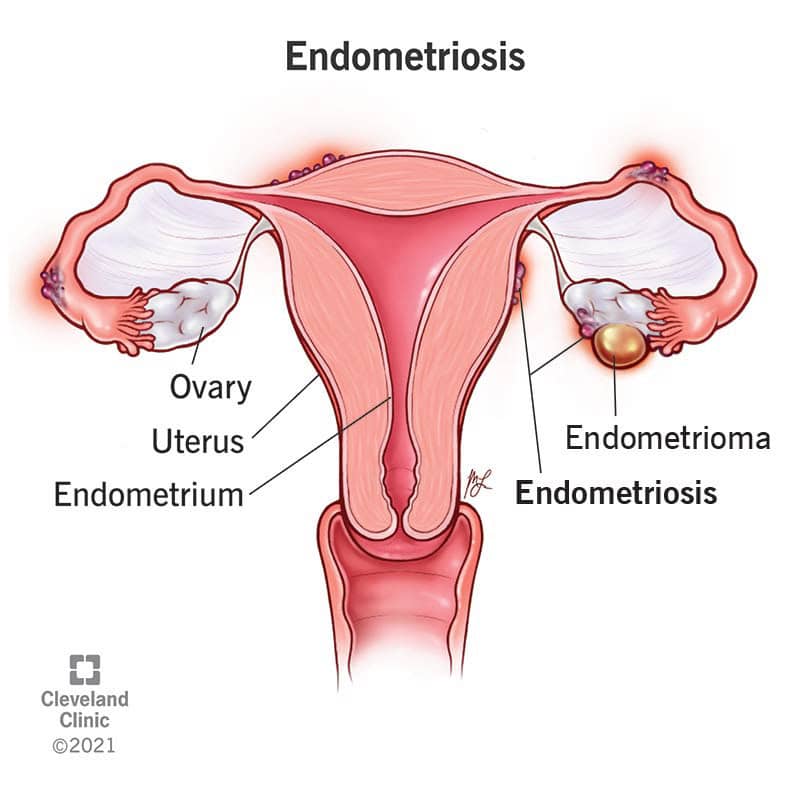
Endometriosis and infertility is a condition in which endometrial tissue that normally lines the inside of the uterus, grows outside the uterus and attaches to the ovaries, fallopian tubes, or other organs in the abdominal cavity. Blood flow from the endometrial tissue is restricted and can cause inflammation and form scar tissue which can block the fallopian tubes or interfere with ovulation with makes it difficult getting pregnant with endometriosis.
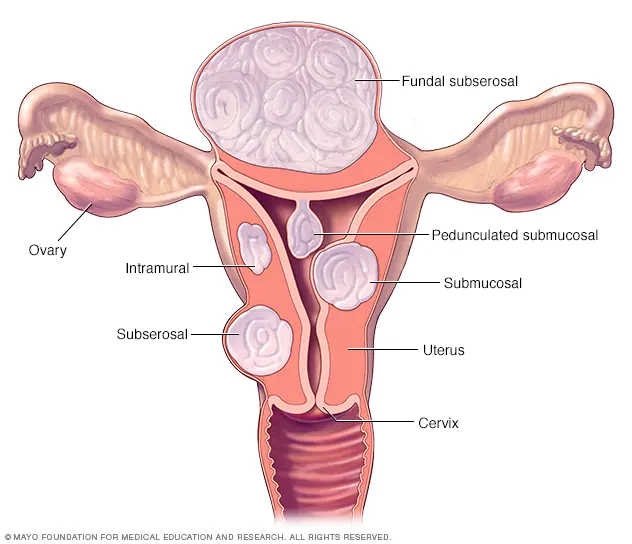
Uterine fibroids, also known as leiomyomas, they can develop from the smooth muscle cells of the uterus and can interfere with pregnancy in many ways. The ones that grow on the inside wall of the uterus can cause changes in the endometrial tissue, making it difficult for a fertilized egg to attach to the uterine wall. Uterine fibroids that develop outside the uterus can interfere with pregnancy by compressing or blocking the fallopian tubes, thereby preventing the sperm from reaching the egg.
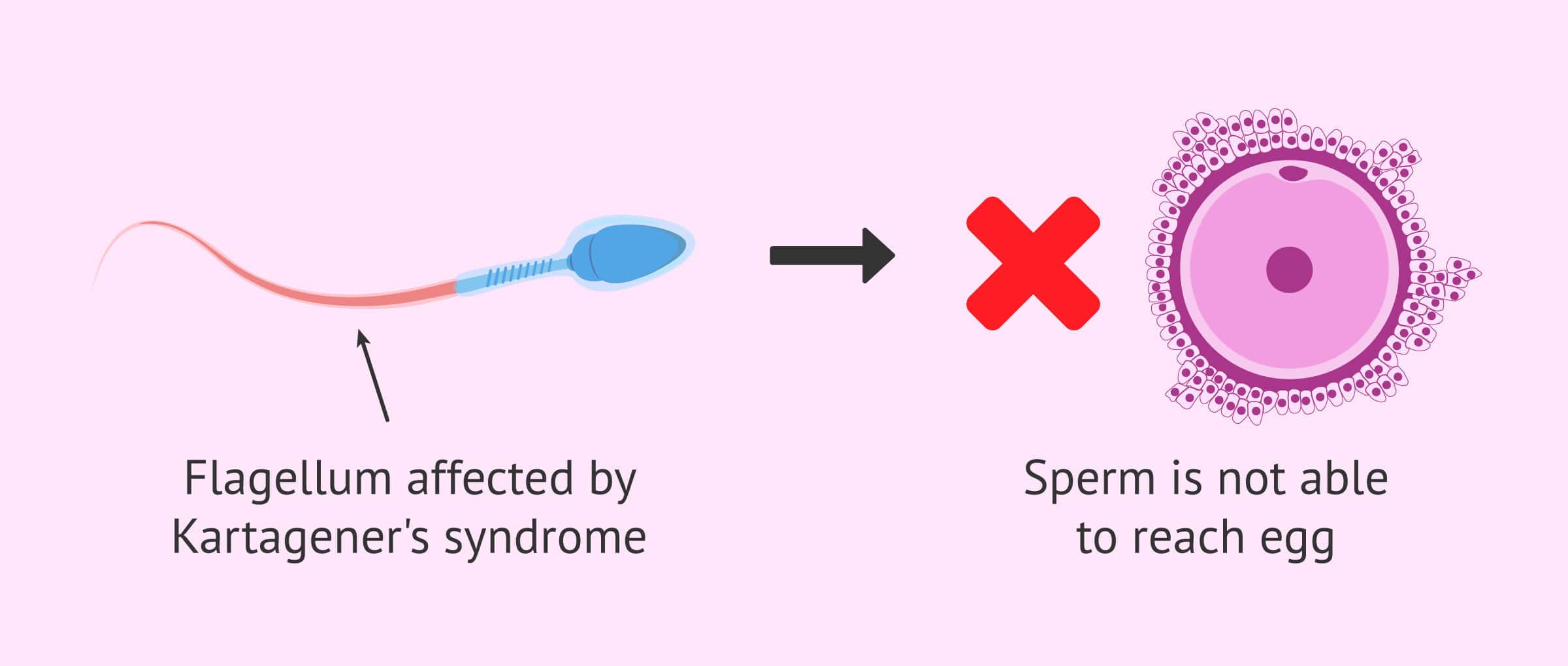
Kartagener syndrome, a rare disorder that is associated with a reversed position of the major organs, also includes immotile cilia (hair-like cells in lungs and sinuses that have a structure similar to the tails of sperm). Germ cells may also be affected by this condition.
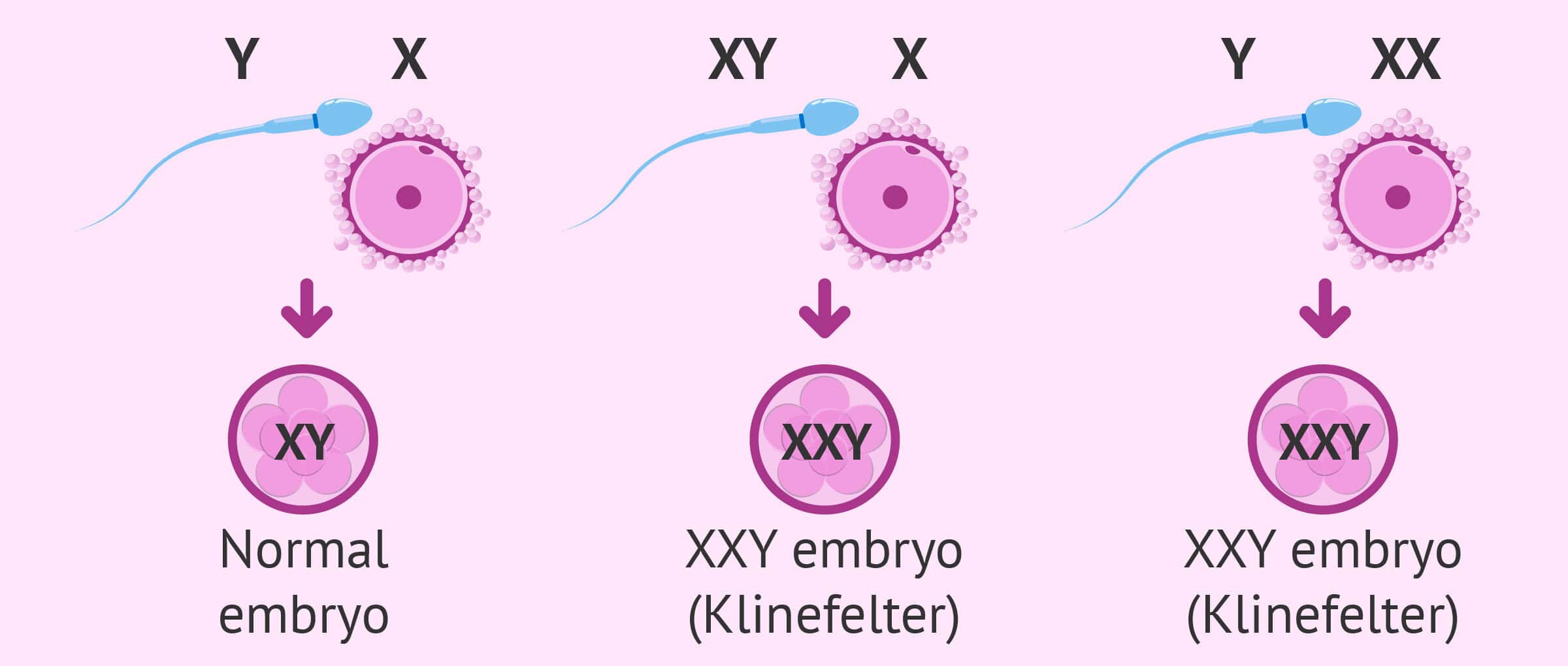
Klinefelter syndrome patients carry two X and one Y chromosomes (the norm is one X and one Y), which leads to the destruction of the lining of the seminiferous tubules in the testicles during puberty, although most other male physical attributes are unimpaired.